This newest addition in our collection of humanized mouse disease models integrates characteristics of the human Systemic Lupus Erythematosus complexity and develops a chronic multiorgan autoimmune disease marked by proteinuria, anti-dsDNA antibodies, severe inflammatory lesions in the skin and milder pathologies in the kidneys and lungs.
This novel model of lupus can prove to be an invaluable translational tool for studying the aetiopathogenic role of the IL23 cytokine in SLE and for use as a preclinical tool to assess the efficacy of novel lupus therapeutics.
Published in Arthritis Rheumatol. 2024 Feb 15. doi: 10.1002/art.42830.
Christodoulou-Vafeiadou E, Geka C, Iliopoulou L, Ntari L, Denis MC, Karagianni N, Kollias G
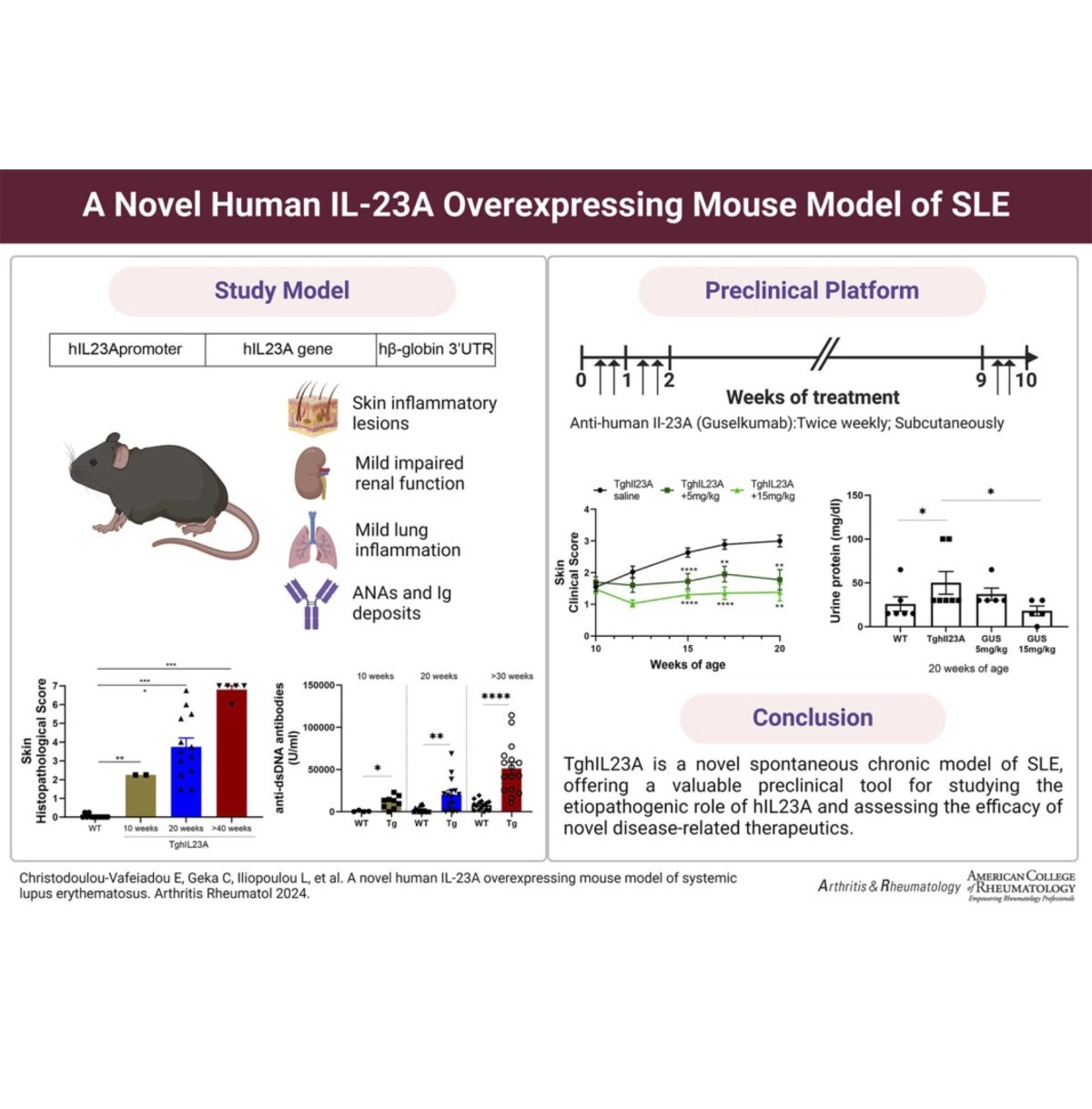
Objective: Interleukin-23 (IL-23) is a crucial cytokine implicated in chronic inflammation and autoimmunity, associated with various diseases like psoriasis, psoriatic arthritis, and systemic lupus erythematosus (SLE). This study aimed to create and characterize a transgenic mouse model (TghIL23A) overexpressing human IL23A, providing a valuable tool for investigating the pathogenic role of hIL23A and evaluating the efficacy of anti-human-IL23A therapeutics.
Methods: TghIL23A mice were generated via microinjection of CBAxC57BL/6 zygotes with a fragment of the human IL23A gene, flanked by its 5′-regulatory sequences and the 3’UTR of human beta-globin. The TghIL23A pathology was assessed through hematological and biochemical analyses, cytokine and anti-nuclear antibody detection, histopathological examination of skin and renal tissues. The response to the anti-hIL23A therapeutic agent guselkumab, was evaluated in groups of 8 mixed-sex mice receiving subcutaneous treatment twice weekly for 10 weeks, using clinical, biomarker and histopathological readouts.
Results: TghIL23A mice exhibited interactions between hIL23A and mouse IL23/IL12p40, and developed a chronic multiorgan autoimmune disease marked by proteinuria, anti-dsDNA antibodies, severe inflammatory lesions in the skin, and milder phenotypes in the kidneys and lungs. The TghIL23A pathological features exhibited significant similarities to those observed in human SLE patients and they were reversed following guselkumab treatment.
Conclusions: We have generated and characterized a novel genetic mouse model of SLE, providing proof-of-concept for the etiopathogenic role of hIL-23A. This new model has a normal lifespan and integrates several characteristics of the human disease’s complexity and chronicity making it an attractive preclinical tool for studying IL23-dependent pathogenic mechanisms and assessing the efficacy of anti-hIL23A or modeled disease-related therapeutics.